Hartley News Online Your alumni and supporter magazine
The notion of assisted suicide is fraught with ethical concerns, not least for the medical profession. Professor Hazel Biggs and Baroness Finlay of Llandaff consider the role that the law and clinicians should play.
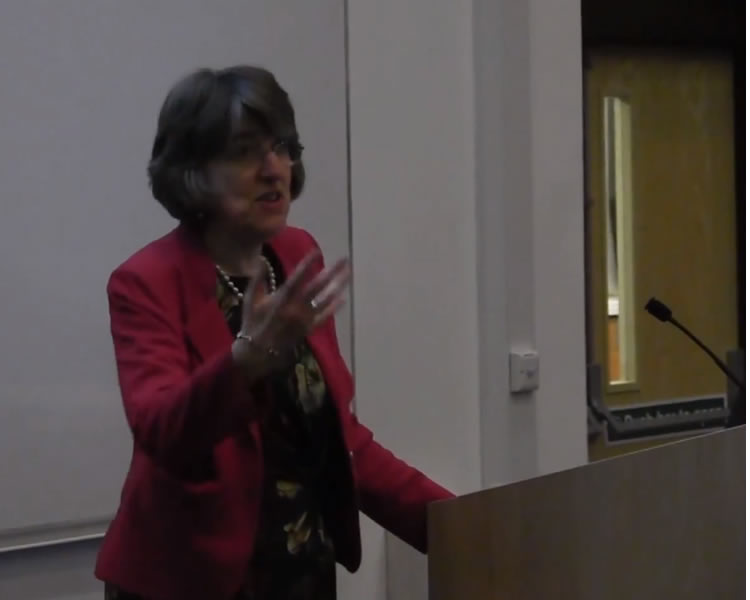
Professor Hazel Biggs, Head of the Southampton Law School: Researchers in Southampton Law School’s Centre for Health Ethics and Law (HEAL) are participating in ethical issues that inform health policy in the UK and globally, and we are particularly influential in the assisted suicide debate.
There’s always something in the press about this issue, whether it’s a legal case in which someone is trying to promote a ‘right to die’, the Director of Public Prosecutions issuing new guidance, or debates in parliament on proposed changes to the law, such as Lord Falconer’s Private Member’s Bill, which is currently making its way through the parliamentary process. We engage with all aspects of the debate; the overarching aim of our work is to lead opinion and raise awareness.
My personal view is that if people are capable of making their own decisions and want to exercise their personal autonomy by being assisted to die, then the law should accommodate that. It is not unlawful to commit suicide, but assisting someone to commit suicide carries a maximum prison sentence of 14 years.
Guidelines issued to the Crown Prosecution Service by the Director of Public Prosecutions in 2010, effectively say that if someone is being assisted to die by a loved one or carer who is not acting in a professional capacity, they are less likely to be prosecuted than someone operating in a professional capacity. That means that doctors and nurses who would have the knowledge to assist someone in a safe way are more likely to be prosecuted. An implication of this is that people may ask carers to help them because professional assistance is not available, which can end up in botched suicide attempts.
We are also witnessing people travelling to jurisdictions where assisted suicide is lawful. Anybody who helps someone travel to these places, for example DIGNITAS in Switzerland, could be prosecuted. We know that there have been more than 200 cases of this, but up until now no prosecutions have been brought.
It would be much more humane to formalise legal guidelines around this issue. One of the problems is that the law isn’t brought in until the assisted suicide has taken place so those who might be vulnerable to being exploited or pressurised are protected only by the threat of criminal prosecution against those who might wish to abuse them. If we formalised it, we could make sure that no one was being pressured into suicide, that it really was their considered wish, and that they were competent to make that decision before any action was taken.
The sanctity of life is obviously a huge issue in this area, and for medical professionals the first imperative is to cure and sustain life. However, the reality is that in some situations this is not possible anymore. The law says that a doctor is entitled to do what is reasonable and proper in circumstances where it is not possible to save a life. So for example it is lawful to provide high doses of pain killers even if it can be anticipated that a side effect could be that the person stops breathing, or in some situations to withdraw life-sustaining treatment even if death will result. Medicine is about caring, but it is not always about curing. It is about keeping people comfortable and making sure that they end their lives in a way that they would wish and where possible, in a way that reflects the values they have lived by.
For more information on Hazel’s work visit www.southampton.ac.uk/heal
Professor Ilora Baroness Finlay of Llandaff, internationally renowned expert in palliative care medicine, chairs the All-Party Parliamentary Group on Dying Well. Baroness Finlay recently presented the University’s Annual Wade Lecture, Dying Well: ‘A right to die’ is a misnomer. We will all die and most medicine today concerns disease control, rather than cure. When disease escapes our treatments to control it, interventions become futile and cease as the person is supported in their dying. But that is fundamentally different in intent and practice from assisting suicide by lethal drugs – irrespective of how long the person might have lived.
We are told by the advocates of assisted suicide that there will be safeguards. But all we have been given are vague conditions – like a settled wish, freedom from pressure or the capacity to make the decision. Yet no minimum requirements have been laid down for meeting those conditions.
For patients to make a valid choice of assisted suicide they need accurate information, they need to have the capacity to take that decision and they need to be free of pressure. So let’s look at each in turn.
Information depends on what the doctor tells the patient. Life expectancy is only a best guess – often the so called terminally ill turn out to live far longer, sometimes years longer, than anyone expected. Diagnostic errors abound. Post-mortems regularly show that around 1 in 20 diagnoses were wrong.
Mental capacity is complex, fluctuates and is difficult to assess. Oregon’s data has shown how often serious impairment is missed in those supplied with a lethal prescription. And as for coercion, no doctor can know what goes on behind closed doors in a family, what finances are at play or who is being made to feel they have a duty to die. I have been taken in – the ‘loving’ husband who persuaded his young dying wife to leave everything to him and write her children out of the will; the ‘loving’ family disappointed because mother outlived her fixed-term life insurance.
Why do people ask to die? Because they fear what lies ahead, particularly feeling they are a burden. Pain is not the issue here – you do not have to kill the patient to kill the pain.
The desire for death fluctuates. It is not fixed. It comes and goes, and is linked to feelings of depression and hopelessness and greatly influenced by the clinician’s attitude. As a Dutch doctor said, “when I suggested euthanasia, patients took that option; when I offer palliative care, patients take that option”. By processing a request to die, the doctor gives the subliminal message: “You’re right – you’d be better off dead. I agree and therefore am processing the request.”
Doctors are very aware of their power and its dangers. They oppose assisting suicide for good reason – as the Royal College of General Practitioners found, 77 per cent of GPs opposed changing the law. In palliative care there is even greater opposition, with only four per cent of specialists prepared to have any involvement in the process. A doctor from Belgium told me that his hospital managers had asked why he hadn’t discussed euthanasia with potentially eligible patients when there was a bed shortage. That kind of pressure endangers good clinical care.
Oregon’s data indicates that over 1,500 patients in England and Wales would prematurely end their lives every year, some by months or years, under the proposals before Parliament. And the numbers are still rising. Of the 20 or so who go to DIGNITAS each year, most don’t fulfil the qualifying criteria in the bills that are being put before Parliament
This debate is a dangerous distraction from relieving distress in the dying. The law that we have now works well. It provides a deterrent against malicious assistance with suicide and it has the discretion not to press charges where it is clear from the evidence that there has been no criminality involved. The law underpins our attitudes to suicide – that, while we treat people who attempt to take their own lives with understanding and compassion, suicide is not something to be encouraged, let alone assisted.
An assisted suicide law sends the message that, for some who are ill, taking your own life is something that you ought to consider. Is this the kind of society into which we want to move?